HTAC Project Summary
What is HTAC?
HTAC is a collaboration between healthcare systems, public health departments, health organizations, and health plans in Minnesota. HTAC uses summary reports from EHRs on a range of chronic, behavioral, and mental health conditions. The information comes from 11 health systems that participate in the Minnesota Electronic Health Record Consortium (MNEHRC). Information from the MNEHRC represents around 90% of healthcare for Minnesotans, which makes HTAC a powerful tool to describe the health of many communities.
HTAC data are updated annually and are available through reports and an interactive dashboard. HTAC reports include:
- Trends in prevalence data (positive or negative changes in the proportion of people with certain diagnoses over time) for high-priority health conditions across the state.
- Health information by patient characteristics (race, ethnicity, language, sex, age, status of experiencing homelessness and incarceration.)
- Data at state, county, zip code and Census tract levels.
How Can Information in HTAC Be Used?
The HTAC health information complements other sources of public health data. HTAC data can be used to:
- Support community health (needs) assessments and community health improvement plans,
- Inform policy and guide local prevention, intervention and response work, and
- Support grant applications.
Who Is Involved?
The HTAC collaboration involves people with great ideas and a passion for creating healthier lives for all Minnesotans. Project partners include the MNEHRC, Hennepin County Public Health, and the Center for Community Health (CCH). Organization and community partners help inform the development of the data dashboard and technical assistance materials.
What Does That Mean?
Electronic Health Record:
Doctors and other healthcare team members mark down conditions discussed and identified during a patient’s visit. Health conditions, test results, and other information are given a code. All of this information is stored in an Electronic Health Record at the office or hospital.
Summary Reports:
Summary reports use information about a group of people. Information about individuals is not used.
Community:
Community can be defined in many ways. A few examples include where people live (geography), shared background (ethnicity), and personal characteristics (such as age and race).
Videos
Health Condition Descriptions
Alcohol Use
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of alcohol use in the last 5 years.
Data notes:
The alcohol use condition includes:
- Alcohol use disorder
- Alcohol intoxication
- Alcohol-induced mental health disorders
- Alcohol-induced organ damage
- Alcohol withdrawal; and
- Other related diagnoses
Anxiety
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of anxiety in the last 5 years.
Data notes:
The anxiety condition includes:
- Generalized anxiety disorder
- Panic disorder
- Social anxiety disorder
- Obsessive-compulsive disorders
- Substance use-related anxiety disorders
- Specific phobias; and
- Other related diagnoses
Arthritis
The prevalence estimates for this condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of arthritis in the last 5 years.
Data notes:
The arthritis health condition includes:
- Osteoarthritis
- Rheumatoid arthritis
- Juvenile arthritis
- Other related diagnoses.
Asthma
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of asthma in the last 5 years.
Data notes:
This condition includes mild to severe asthma, asthma attacks, and other related diagnoses.
Bipolar Disorder
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of bipolar disorder in the last 5 years.
Data notes:
The bipolar disorder condition includes:
- Bipolar I disorder
- Bipolar II disorder
- Cyclothymic disorder; and
- Other related diagnoses
Cancer
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health systems within the last 3 years and received a diagnosis of cancer in the last 5 years.
Data notes:
The cancer health condition includes any cancer diagnosis except for non-melanoma skin cancer.
Cannabis Use
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of cannabis use in the last 5 years.
Data notes:
The cannabis use condition includes:
- Cannabis use disorder
- Cannabis overdose (accidental or intentional)
- Cannabis intoxication
- Cannabis-induced mental health disorders; and
- Other related diagnoses
Chronic Kidney Disease (CKD)
The prevalence estimates for this condition include Minnesota residents who were seen at any participating health system within the last 3 years and:
a) received a diagnosis of chronic kidney disease in the last 5 years.
b) has a most recent outpatient estimate glomerular filtration rate less than 60, or
c) has a most recent urine albumin to creatinine ratio equal to or greater than 30.
Data Notes:
This condition includes chronic kidney disease, kidney failure, and other related diagnoses.
Chronic Obstructive Pulmonary Disorder (COPD)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of COPD in the last 5 years.
Data notes:
This condition includes:
• COPD
• Emphysema
• Chronic bronchitis; and
• Other related diagnoses
Cocaine Use
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of cocaine use in the last 5 years.
Data notes:
The cocaine use condition includes:
- Cocaine use disorder
- Cocaine overdose (accidental or intentional)
- Cocaine intoxication
- Cocaine withdrawal
- Cocaine-induced mental health disorders; and
- Other related diagnoses
Deliveries
The prevalence estimates for this condition include obstetrical deliveries where, at the time of the delivery, the patient was:
- Female
- 12-55 years old
- A Minnesota resident; and
- Had a delivery hospitalization at a participating health system during a given year.
Data note: Prevalence estimates for deliveries are calculated as a percentage of deliveries among people who could give birth rather than among the whole population.
Depression
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of depression in the last 5 years.
Data notes:
The depression condition includes:
• Major depressive disorder
• Single depressive episodes
• Postpartum depression; and
• Other related diagnoses
Diabetes (Type 2)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of type 2 diabetes or one A1c measure > 6.5 in the last 5 years.
Data notes:
- This condition includes:
- Type 2 diabetes
- Disorders and complications caused by diabetes; and
- This condition does not include type 1 diabetes diagnoses and complications
Hallucinogen Use
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of hallucinogen use in the last 5 years.
Data notes:
- The hallucinogen use condition includes:
- Hallucinogen use disorder
- Hallucinogen overdose (accidental or intentional)
- Hallucinogen intoxication
- Hallucinogen-induced mental health disorders; and
- Other related diagnoses
- Diagnoses are related to hallucinogens such as LSD, peyote, psilocybin, or PCP
Heart Attack (Acute Myocardial Infarction)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of acute myocardial infarction in the last 5 years.
Data notes:
- The acute myocardial infarction condition includes:
- Heart attacks
- Chest pain and other complications due to heart attack;
- Other related diagnoses
Heart Disease (Ischemic Heart Disease)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of ischemic heart disease in the last 5 years.
Data notes:
- The ischemic heart disease condition includes:
- Chronic heart disease
- Acute heart disease
- Coronary heart disease
- Atherosclerosis
Heart Failure
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of heart failure in the last 5 years.
Data notes:
This condition includes:
• Acute and chronic heart failure
• Rheumatic heart disease
• Cardiomyopathy; and
• Other related diagnoses
Hyperlipidemia (High Cholesterol)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of high cholesterol in the last 5 years.
Data notes:
This condition includes hyperlipidemia and related diagnoses.
Hypertension (High Blood Pressure)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of high blood pressure or any two BP >=140/90 in the last 3 years for hypertension on two different days in the last 5 years.
Data notes:
This condition includes hypertension, resulting complications, and other related diagnoses.
Inhalant Use
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of inhalant use in the last 5 years.
Data notes:
The inhalant use condition includes:
• Inhalant use disorder
• Inhalant overdose (accidental or intentional)
• Inhalant intoxication
• Inhalant-induced mental health disorders; and
• Other related diagnoses
Lung Cancer
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of lung cancer in the last 5 years.
Data Notes:
The lung cancer condition includes:
- History of lung cancer
- Maignanct neoplasm of bronchus or lung
- Malignant carcinoid tumor of the bronchus or lung
- Carcinoma in situ of bronchus or lung
This condition also includes different types and severity of lung cancers and other related diagnoses.
Maternal Opioid Use
The prevalence estimates for this health condition include deliveries where, at the time of delivery, the patient was:
- Female
- 12-55 years old
- A Minnesota resident
- Had a delivery hospitalization at a participating health system during a given year; and
- An opioid use-related diagnosis was noted at the time of delivery.
Data Notes:
Opioid Use includes:
- Opioid use disorder
- Opioid overdose (accidental or intentional)
- Opioid intoxication
- Opioid-induced mental health disorders
- Opioid withdrawal, and
- Other related diagnoses
Diagnoses are related to a range of opioids such as opioid medicines, opium, methadone, heroin, and fentanyl.
Prevalence estimates for maternal opioid use are calculated as a percentage of maternal opioid use among all deliveries rather than among the whole population.
Obesity
The prevalence estimates for this condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of obesity OR had a documented body mass index (BMI) of greater than 30 in the last 5 years.
Data Notes:
- This condition includes overweight, obesity, obesity-related maternal health complications, and other related diagnosis.
- Obesity is limited to 18+ because weight percentiles are used for children.
Opioid Use
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of opioid use in the last 5 years.
Data notes:
- The opioid use condition includes:
- Opioid use disorder
- Opioid overdose (accidental or intentional)
- Opioid intoxication
- Opioid-induced mental health disorders
- Opioid withdrawal; and
- Other related diagnoses
- Diagnoses are related to a range of opioids such as opioid medicines, opium, methadone, heroin, and fentanyl
Pediatric Obesity
The prevalence estimates for this health condition include Minnesota residents aged 2-17 who were seen at any participating health system within the last 3 years and had a documented body mass index (BMI) measurement indicating pediatric obesity in the last 5 years.
Data notes:
- Prevalence estimates for pediatric obesity are based on BMI measurement and do not account for diagnoses.
- This condition includes patients whose most recent BMI measurement was within the 95th percentile or above for their age and sex.
Peripheral Vascular Disease (PVD)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of peripheral vascular disease in the last 5 years.
Data notes:
This condition includes peripheral vascular diseases and PVD-related pain, tissue damage, and other complications.
Post-Traumatic Stress Disorder (PTSD)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of PTSD in the last 5 years.
Data notes:
The PTSD condition includes acute and chronic post-traumatic stress disorders.
Psychostimulant Use
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of psychostimulant use in the last 5 years.
Data notes:
- The psychostimulant use condition includes:
- Psychostimulant use disorder
- Psychostimulant overdose (accidental or intentional)
- Psychostimulant intoxication
- Psychostimulant withdrawal
- Psychostimulant-induced mental health disorders; and
- Other related diagnoses
- Diagnoses are related to psychostimulants such as methamphetamines, ecstasy, or MDMA
Psychotic Disorders
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of a psychotic disorder in the last 5 years.
Data notes:
The psychotic disorders indicator includes:
• Schizophrenia
• Paranoia
• Postpartum psychosis
• Schizoaffective disorder, and
• Other related diagnoses
Sedative Use
The prevalence estimates for this indicator include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of sedative use in the last 5 years.
Data notes:
- The sedative use indicator includes:
- Sedative use disorder
- Sedative overdose (accidental or intentional)
- Sedative intoxication
- Sedative-induced mental health disorders; and
- Other related diagnoses
- Diagnoses are related to sedatives such as benzodiazepines, barbiturates, and hypnotics
Severe Maternal Morbidity
The prevalence estimates for this health condition include deliveries where, at the time of delivery the patient was:
- Female
- 12-55 years old
- A Minnesota resident
- Had a delivery hospitalization at a participating health system during a given year; and
- A severe maternal morbidity diagnosis was attached to the delivery.
Data notes:
The severe maternal morbidity condition includes a range of negative health outcomes of labor and delivery that have short- and long-term health consequences. For example, complications from infection, anesthesia, and surgery resulting in events like heart attack, stroke, aneurysm, embolism, hemorrhage, and more.
Prevalence estimates for severe maternal morbidity are calculated as a percentage of severe maternal morbidity events among all deliveries rather than among the whole population.
Severe Pediatric Obesity
The prevalence estimates for this health condition include Minnesota residents aged 2-17 who were seen at any participating health system within the last 3 years and had a documented body mass index measurement indicating severe pediatric obesity in the last 5 years.
Data notes:
- Prevalence estimates for pediatric obesity are based only on BMI measurement, and do not account for diagnoses.
- This condition includes patients whose most recent BMI masurement was at least 120% of the 95th percentile for their age and sex.
Stroke
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of a stroke in the last 5 years.
Data notes:
The stroke indicator includes:
- Ischemic stroke
- Transient ischemic attacks (also called TIA or mini-stroke)
- Brain bleed
- Other effects and complications of reduced blood flow to the brain; and
- Other related diagnoses
Suicidal Ideation or Recent Attempt
The prevalence estimates for this condition include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of suicidal ideation or attempt in the last 5 years.
Data notes:
- The suicide condition includes:
- Suicidal thoughts
- Intentional self-harm
- Suicide attempts
- Suicidal ideation accounts for most of this condition’s prevalence estimates. Intentional self-harm accounts for a small portion.
Health Condition Group Descriptions
Any Cardiovascular Condition
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of a condition that increases the chance of developing a cardiovascular disease (risk factor).
Data note:
Cardiovascular risk factor conditions include:
- Diabetes, Type II
- Acute Myocardial Infarction (heart attack)
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease
- Stroke
- Chronic Kidney Disease
Any Mental Health Condition
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a mental health condition diagnosis in the last 5 years.
Data Note:
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
Any Mental Health Condition or Substance Use Disorder
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a mental health condition diagnosis or a substance use disorder diagnosis in the last 5 years.
Data Note:
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Any Physical Health Condition
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received any physical health condition diagnosis in the last 5 years.
Data Note:
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
Any Substance Use Disorder
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a substance use disorder diagnosis in the last 5 years.
Data Note:
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Both Mental Health Condition and Substance Use Disorder Diagnosis
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a mental health condition diagnosis and a substance use disorder diagnosis in the last 5 years.
Data Note:
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Cardiovascular Health Condition and Mental Health Condition
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of a condition that increases the chance of developing a cardiovascular disease (risk factor) and a mental health condition disorder diagnosis in the last 5 years.
Data note:
Cardiovascular risk factor conditions include:
- Diabetes, Type II
- Acute Myocardial Infarction (heart attack)
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease
- Stroke
- Chronic Kidney Disease
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
Cardiovascular Health Condition And Mental Health Condition or Substance Use Disorder
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of a condition that increases the chance of developing a cardiovascular disease (risk factor) and a mental health condition diagnosis or substance use disorder diagnosis in the last 5 years.
Data note:
Cardiovascular risk factor conditions include:
- Diabetes, Type II
- Acute Myocardial Infarction (heart attack)
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease
- Stroke
- Chronic Kidney Disease
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Cardiovascular Health Condition and Substance Use Disorder
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a diagnosis of a condition that increases the chance of developing a cardiovascular disease (risk factor) and a substance use disorder diagnosis in the last 5 years.
Data note:
Cardiovascular risk factor conditions include:
- Diabetes, Type II
- Acute Myocardial Infarction (heart attack)
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease
- Stroke
- Chronic Kidney Disease
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Physical Health Condition (2 diagnoses)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received 2 physical health condition diagnoses in the last 5 years.
Data Note:
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
Physical Health Condition (3+ diagnoses)
The prevalence estimates for this health condition include Minnesota residents who were seen at any participating health system within the last 3 years and received 3 or more physical health condition diagnoses in the last 5 years.
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
Physical Health Condition and Mental Health Condition
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a physical health condition diagnosis and a mental health condition diagnosis in the last 5 years.
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
Physical Health Condition and Mental Health Condition or Substance Use Disorder
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a physical health condition diagnosis and a mental health condition diagnosis, or a substance use disorder diagnosis in the last 5 years.
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Physical Health Condition and Substance Use Disorder
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a physical health condition diagnosis and a substance use disorder diagnosis in the last 5 years.
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Physical Health Condition, Mental Health Condition, and Substance Use Disorder
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received a physical health condition diagnosis and a mental health condition diagnosis, and a substance use disorder diagnosis in the last 5 years.
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Substance Use Disorder (2 substances)
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received 2 substance use disorder diagnoses in the last 5 years.
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Substance Use Disorder (3+ substances)
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received 3 or more substance use disorder diagnoses in the last 5 years.
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Two Or More Conditions (Any)
The prevalence estimates for this health condition group include Minnesota residents who were seen at any participating health system within the last 3 years and received 2 or more of any cardiovascular risk factor condition, physical health condition, mental health condition, or substance use disorder diagnosis.
Data note:
Cardiovascular risk factor conditions include:
- Diabetes, Type II
- Acute Myocardial Infarction (heart attack)
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease
- Stroke
- Chronic Kidney Disease
The physical health condition diagnoses include:
- Asthma
- Chronic Kidney Disease (CKD)
- Chronic Obstructive Pulmonary Disease (COPD)
- Diabetes, Type II
- Acute MI (heart attack)
- Heart failure
- Hyperlipidemia
- Hypertension
- Peripheral Vascular Disease (PVD)
- Stroke
- Arthritis
- Cancer
The mental health condition diagnoses include:
- Anxiety disorders
- Bipolar disorders
- Depressive disorders
- Post-Traumatic Stress Disorder (PTSD)
- Psychotic disorders
- Suicidal ideation
The substance use disorder condition diagnoses include:
- Alcohol use
- Cannabis use
- Cocaine use
- Hallucinogen use
- Inhalant use
- Opioid use
- Psychostimulant use
- Sedative use
- Any other substance use
Glossary of Technical Terms
Adjusted vs. unadjusted data
Differences in characteristics between groups, such as age and sex, may influence the prevalence of certain health conditions. Adjusting is a statistical process that helps compare the rates of health conditions when these differences occur. Adjusted rates take into consideration these differences. Unadjusted rates use the actual (“raw”) prevalence of health conditions without taking age and sex differences into account. The HTAC dashboard shows both adjusted and unadjusted rates of health conditions.
Denominator
For a prevalence rate, the denominator is the entire defined population. For HTAC, the population is based on the number of EHR records from healthcare systems included in the MN EHR Consortium.
Electronic Health Record (EHR)
An electronic health record (EHR) is an electronic version of a patient’s medical chart. During a visit with a patient, healthcare staff enter health information such as diagnoses, vital signs, demographics, lab data, immunizations, medications, notes, and more.
Health disparity
Health disparities are differences in health among population groups based on characteristics like sex, race, ethnicity, neighborhood, or geographic location.
Homelessness Experience
Homelessness experience includes Minnesota Homeless Management Information System (HMIS) records consistent with the use of emergency shelter beds, street outreach services, transitional housing, or supportive housing during 2024.
Lookback period
A lookback period is the timeframe from which data are included in the analysis. For HTAC, the lookback period includes data for people who were seen at a participating health system within the last 3 years and received a diagnosis related to one of the featured health conditions within the last 5 years.
Numerator
A numerator is a subset of the people included in the denominator. For a prevalence rate, the numerator is the number or count of people in the population with the health condition of interest. For example, if 3000 people have the condition of interest and the total defined population is 15,000, the numerator is 3,000.
Prevalence
The percentage of people in the population with a certain health condition. For example, if 3000 people have the condition of interest and the total defined population is 15,000, people then the prevalence is 20% (3,000/15,000 = .20).
Social Vulnerability Index (SVI)
Social Vulnerability Index (SVI) is a commonly used tool for public health planning and emergency preparedness. SVI is used to help predict how at-risk a community is to natural disasters, epidemics, climate change, and other public health emergencies. The SVI takes into consideration several factors, such as community poverty levels, types of housing, household characteristics, and more.
Summary data
Summary (or aggregated) data combines information on individuals to create a group total so that we can understand the health of a whole community while maintaining confidentiality.
Frequently Asked Questions
What is Health Trends Across Communities?
Health Trends Across Communities (HTAC) is a unique collaboration of health systems, local public health departments, and health plans. Our goal is to promote health equity and improve the health of communities across Minnesota by providing accessible, timely, and detailed health information.
How can HTAC reports be used?
HTAC reports can help users understand the health and well-being of our communities. HTAC provides summary reports on the prevalence of multiple health conditions (Prevalence refers to the proportion of people with certain diagnoses.) There are many potential ways this information can be used, including community health assessments, collaborations between different organizations and agencies, grant writing, program planning, evaluation, and more.
HTAC reports can help users:
- Explore and visualize the prevalence of a health condition by demographic characteristics (such as age, race, and ethnicity) and geographic area (such as census tract, city, county, and statewide across Minnesota)
- Examine health disparities within and across communities
- Track community-level health outcomes and behaviors over time
- Decide how and where to target resources and programs
- Advocate for the resources that their community needs
- Develop policies and evaluate their impact
Where does HTAC information come from?
HTAC uses summary reports from electronic health records from participating health systems to estimate the proportion of people with different health conditions. HTAC includes information from:
- Hospitalizations
- Emergency department visits
- Health diagnosis (ICD-10) codes
- Medical procedures
- Laboratory values
- Medications
- Other healthcare encounter information
HTAC also includes information about:
- Demographic characteristics (age, race ethnicity, etc.)
- Location (state, region, county, city, and census tract)
- Social determinants of health (homelessness, incarceration, and Medicaid enrollment)
- Social Vulnerability Index
- Deaths
Who is represented in the reports?
HTAC reports are maintained by the Minnesota Electronic Health Record Consortium (MNEHRC), which is a collaboration between Minnesota’s 11 largest health systems, local public health agencies, state homelessness and correctional agencies, researchers, clinicians, and Minnesota Department of Health representatives. As a result of this expansive partnership, information from the MNEHRC represents health care for around 90% of Minnesotans.
HTAC reports provide estimates of the proportion of people with certain health conditions among people who received care at a participating health system. People are included if they are a Minnesota resident and received care at least once at any of the participating health systems within the reporting period.
Who can use HTAC reports?
HTAC dashboards are free to access and open to the public. Users might include local public health departments, health systems, nonprofits, social service organizations, students, health advocates, and community organizations.
Why use electronic health record data for community health?
Information from electronic health records (EHRs) can provide unique insights into the health of communities.
EHRs have several strengths as a data source:
- The data has already been collected. It does not rely on people responding to surveys.
- The data is current.
- The data can provide detailed information on health by race, sex, age, geography, and more.
- For HTAC, the data represents a large portion of the state population. HTAC information from the MNEHRC represents health care for approximately 90% of Minnesotans.
What are the limitations of electronic health record data?
As with all data sources, summary reports from electronic health records have limitations. Users should keep these limitations in mind when interpreting the reports.
Limitations include:
- The 11 largest health systems in Minnesota participate in HTAC. Information represents health care for approximately 90% of Minnesotans. However, not all health systems and health services in the state participate in HTAC and provide summary information.
- The reports only include people who received health care at one of the participating health systems.
- The reports only include people who receive health care within a certain timeframe.
- For some conditions, the reporting relies on people disclosing certain health behaviors, such as substance use.
- Clinical information is collected by health systems mainly for billing or patient care, not for community health.
- When entering patient information into an EHR, a healthcare provider may make an error or not complete certain information, especially if it’s not required. This could lead to issues with quality.
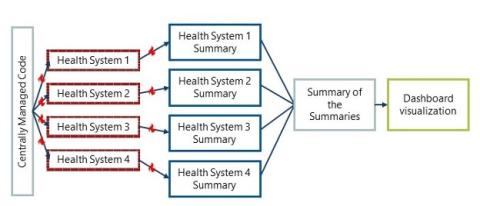
How is patient privacy protected?
HTAC information does not identify patients and does not include protected health information. All data about individual patients stays within each health system’s secure system. The MNEHRC does NOT access individual medical records.
Each health system generates a summary report that is combined with summaries from other health systems. Individual health system data is not shared. HTAC users only have access to the summary combined information. Sharing only summary information allows for patient privacy to be maintained.
Also, information is not reported if fewer than 11 people have a particular condition in a census tract. This policy helps protect patient confidentiality.
Who are the project partners?
This project is led by a partnership of the Minnesota Electronic Health Record Consortium, the Center for Community Health (CCH), and Hennepin County Public Health.
HTAC reports are built and maintained by the Minnesota Electronic Health Record Consortium (MNEHRC), which is a collaboration between Minnesota’s 11 largest health systems, local public health agencies, state homelessness and correctional agencies, researchers, clinicians, and Minnesota Department of Health representatives. As a result of this expansive partnership, the reports represent health care for at least 90% of Minnesotans.
MNEHRC provides overall project leadership, leads community engagement, and coordinates data management, analysis, and reporting among partners.
Eleven MNEHRC members participate in the HTAC project and provide time, resources, and summary health information:
- Allina Health
- CentraCare
- Children's Minnesota
- HealthPartners
- Essentia Health
- Hennepin Healthcare
- M Health Fairview and the University of Minnesota
- Mayo Clinic and Mayo Clinic Health System
- Minneapolis VA Health Care System
- North Memorial
- Sanford Health
The Center for Community Health (CCH) provides broad direction setting for the project.
Hennepin County Public Health is the fiscal agent, supports project management, and builds project-related communications and technical capacity.
Minnesota Department of Health's Center for Public Health Practice funds this pilot project through a Minnesota Public Health Infrastructure Grant.
A healthcare provider in my county or area is not part of a health system participating in the MN EHRC. How should I interpret data in my county or area?
Prevalence information is generally reliable across regions in Minnesota, even if a health system in a given area does not contribute to HTAC.
First, HTAC data include many people who do not regularly get their care directly through a participating health system. Some healthcare providers participate in HTAC through a larger healthcare system's electronic health record. Even people who do not regularly receive care through a participating healthcare system in a three year period.
Second, HTAC's population coverage is much better than any other health resource. Compared to census figures, we estimate that many areas of the state represent more than 90% of the population. Even in places where coverage is lower, people from your community who are represented in the data are likely similar to those who are not, allowing for reasonable prevalence estimates. In areas where a major healthcare provider does not participate in HTAC, we encourage data users to use prevalence information rather than the specific number of people with a condition (count).
Please reach out to mnehrc@hhrinstitute.org or the participating healthcare systems in your area for additional information.
How were these health conditions chosen?
The Minnesota Electronic Health Record Consortium (MNEHRC) and the Center for Community Health’s Assessment Alignment Committee (AAC) collaborated to select the initial list of over 20 health conditions that are currently reported on the HTAC dashboard.
First, the MNEHRC reviewed 45 potential health conditions and outcomes for the following criteria:
- Available in EHR
- High enough prevalence to be reported
- Ability to analyze and report by race, ethnicity, and geography
- Data is available for all jurisdictions
Then, the Center for Community Health’s Assessment Alignment Committee members scored and ranked this list of health conditions using the following criteria:
- Has public health significance
- Potential for action through public health interventions
- Existing information is not readily available or has major limitations
- Is an emerging condition or state
- Has alignment with current public health priorities
- EHR data could provide detailed information to support assessment work
Current health conditions included:
- Alcohol Use
- Anxiety
- Asthma
- Arthritis
- Bipolar Disorder
- Cannabis Use
- Cancer
- Cocaine Use
- COPD
- Dementia
- Depression
- Diabetes (Type 2)
- Gun Violence
- Hallucinogen Use
- Heart Failure
- Hyperlipidemia
- Hypertension
- Inhalent Use
- Lung Cancer
- Opioid Use
- Pediatric Obesity
- Post-Traumatic Stress Disorder (PTSD)
- Psychostimulant Use
- Psychotic Disorder
- Sedative Use
- Suicidal Ideation or Attempt
What technical infrastructure does HTAC use?
HTAC’s technical infrastructure was developed and is maintained by the Minnesota Electronic Health Record Consortium (MNEHRC). This infrastructure is based on a distributed data approach. In a distributed data model, the detailed data stays within the health system and is not shared. Health systems share summary information, such as counts of people with certain conditions (which does not identify any individual patient). The summary information from each health system is centrally combined and analyzed.
Sharing summary information is made possible through using a common format, often called a common data model, at each participating health system. The MNEHRC uses a common data model called the Observational Medical Outcomes Partnership (OMOP).
Data analysts create the HTAC dashboards using a software program called Power BI.
Are people who use multiple health systems counted more than once?
No. The Minnesota Electronic Health Record Consortium (MNEHRC) uses a one-way encryption process to deduplicate across health systems. This means that information for a given patient will be included in only one health systems summary report, even if the person has received care at more than one health system.
Why are some census tracts blank?
Estimates are hidden if there are fewer than 11 people with a particular condition. This helps protect patient confidentiality. This policy is called data suppression and follows the Center for Medicaid and Medicare Service’s policy.
How do you determine how many people have a particular condition?
We include anyone who was diagnosed with a condition in the last five years and was seen at a participating health system within the last three years.
Why do you only include people who have been seen at a participating health system in the last three years?
A standard among health systems is to think about panels of patients who have been seen in the last three years. In addition, when people who are seen in the more distant past are included, the likelihood of including people who have moved out of state increases.
Are people who died included?
No. For chronic conditions (e.g., diabetes), people who died before December 31 of the reporting year are excluded. This way, we report the prevalence of conditions among individuals alive on December 31 of a given year. For event-based conditions (e.g., maternal morbidity), people who died before January 1 of the reporting year are excluded. This way, we report the incidence rate for individuals at risk of having an event on January 1 of the reporting year.
How should I cite information in the HTAC dashboard?
Minnesota Electronic Health Record Consortium. “Health Trends Across Communities in Minnesota.” [Date accessed]. https://mnehrconsortium.org/health-trends-across-communities-minnesota-dashboard
Can I download the data from HTAC for use in my study, community health assessment, grant application, etc?
Yes! Please complete this HTAC Public Use Data Request to submit a request to access the data. The purpose of this survey is to collect information that will assist us in monitoring the appropriate use of HTAC data. We will review your response shortly and send you the public use file or a request for more information.
Who can I contact to learn more?
Reach out to MNEHRC@hhrinstitute.org for more information about this project.